In most healthcare teams, dysfunction doesn’t announce itself with shouting matches or dramatic confrontations. It enters quietly, one avoided conversation at a time. The problem isn’t usually that people argue too much. It’s that they stop arguing at all. Silence settles in. Decisions become performative. Accountability fades. Results start to suffer.
If you lead in healthcare, especially as a nurse leader, you’ve likely seen this unfold. A team meeting ends with nods all around, but no action follows. A nurse agrees to a plan during huddle, then does something else entirely. A manager says their door is always open, but staff stop walking through it. The issue isn’t disorganization. It’s that it’s no longer safe to disagree.
To build better teams, we need to understand how high-performing units quietly slip into dysfunction. The truth is, most breakdowns aren’t caused by bad intentions. They’re caused by subtle cultural drift. And that drift shows up in five key patterns:
Guarded becomes Candid
Vague becomes Anchored
Detached becomes Accountable
Artificial becomes Constructive
Fractured becomes Unified
These aren’t just opposites. They’re cultural shifts. Each one influences the others. When trust breaks down, clarity follows. Without clarity, ownership disappears. Without ownership, healthy disagreement dies. And without disagreement, unity becomes fragile.
Let’s unpack each shift and explore what leadership can do to rebuild team strength.
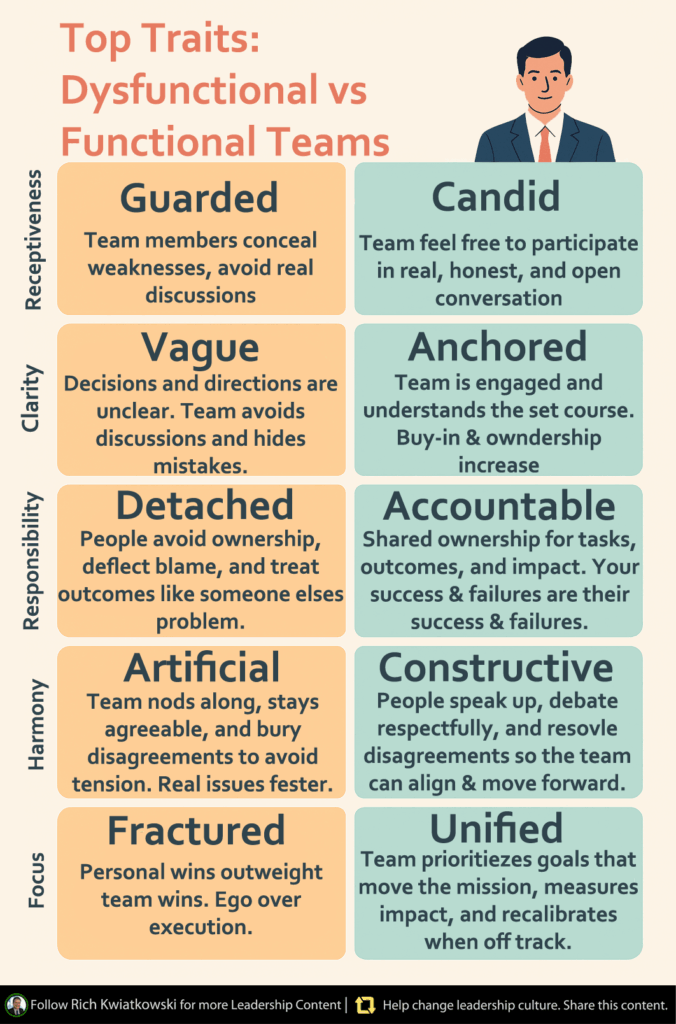
Guarded vs Candid: Creating Real Psychological Safety
When teams become guarded, vulnerability disappears. People stop saying what they really think. They hide mistakes. They stay quiet in meetings even when they see a problem. And eventually, they stop contributing anything beyond the minimum.
This doesn’t always look like fear. It often looks like politeness. Nurses nod, smile, and keep working. But underneath, they don’t trust that their voice is safe. They may have been dismissed before. Or worse, punished for speaking up.
Candid teams are different. They make space for imperfection. People admit mistakes, ask questions, and raise concerns without fear of retribution. Trust builds in those small moments when someone says, “I don’t know,” and is met with support, not judgment.
In high-pressure environments like hospitals, this kind of candor isn’t optional. It’s the foundation of safety and adaptability. A team that hides its struggles cannot improve. But a team that shares them early can solve problems before they grow.
Leaders can create this safety by going first. Admit where you’re unsure. Say what you missed. Celebrate the person who challenges the plan for the sake of patient care. And above all, reward honesty even when it makes things harder in the moment.
Vague vs Anchored: Bringing Clarity to Chaos
Trust alone won’t keep a team aligned. Without clarity, even high-trust teams can drift. In vague teams, meetings end without clear decisions. Roles are blurry. Directions change depending on who you ask. People nod in agreement, but walk away confused.
In healthcare, where timing and precision matter, vague communication can cost lives. It leads to duplicated work, missed cues, and frustrated staff who feel like they’re failing despite trying hard.
Anchored teams solve this by locking in clarity. After each discussion, there’s a shared understanding of what was decided, who owns what, by when, and why. That clarity anchors execution.
Instead of long protocols, anchored teams often use simple habits. They recap decisions aloud. They assign ownership explicitly. They confirm next steps in writing. In chaotic settings like hospitals, these practices cut through overwhelm.
Leaders don’t need to micromanage every detail. But they do need to model clarity. End every meeting with a summary. Make expectations visible. Repeat yourself more than you think you should. And when in doubt, assume your message wasn’t clear and clarify again.
Get our 2025 Nurse Salary Guide
Detached vs Accountable: Rebuilding Shared Ownership
When teams become detached, work gets done by inertia, not intention. Everyone assumes someone else is responsible. Small issues grow into big ones because no one feels ownership. Feedback becomes rare. The gap between intention and outcome widens.
Detachment often feels safe. If I don’t own it, I can’t be blamed. But in practice, it leaves patients underserved and teams demoralized.
Accountable teams flip the script. Ownership is shared, not assigned. People speak up when standards slip. They hold each other to agreements. Feedback flows sideways, not just downward. They care about the outcomes, not just the tasks.
In healthcare, shared accountability is what keeps care plans from falling through the cracks. It’s what makes the difference between catching an error and reporting one. And it starts with leadership.
Leaders should normalize peer feedback. Encourage staff to check in with each other, not just escalate to you. Create space for honest reflection, not just performance reviews. And when something fails, ask, “What was our part in this?” not just “Who dropped the ball?”
Artificial vs Constructive: Turning Conflict into Collaboration
It may sound strange, but not fighting is often a red flag. Teams that never disagree aren’t usually aligned. They’re often suppressing tension. And when conflict goes underground, it shows up as gossip, withdrawal, or passive resistance.
Artificial harmony is quiet on the surface, but corrosive underneath. Constructive teams, on the other hand, argue well. They challenge ideas early. They resolve tensions openly. They disagree with respect and move forward with clarity.
In healthcare, this kind of conflict is vital. Disagreements about care plans, safety concerns, or staffing issues need to be addressed early, not buried. Constructive conflict prevents harm.
To lead this kind of team, set clear norms. Make it safe to challenge decisions. Model how to debate ideas without attacking people. And always close conflict with resolution, not avoidance.
Curious what a top-down, culture-first search could do for your unit? Schedule a call today
Fractured vs Unified: Choosing Mission Over Ego
In fractured teams, everyone chases their own wins. Units compete instead of collaborate. Staff focus on personal success, not patient outcomes. Communication breaks down. Resources are hoarded. Recognition is uneven.
But unified teams share purpose. They measure success collectively. They adjust when someone struggles. They see wins as team efforts, not individual victories.
In hospitals, where care is coordinated and continuous, unity isn’t just idealistic. It’s essential. Disconnected teams drop patients during transitions. They duplicate work. They burn out faster.
Unity starts when leaders model mission focus. They ask questions like, “How does this serve the patient?” They celebrate collective progress. And they make sure no team becomes the hero at the expense of another.

Why Feedback Feels Like a Threat
All of this ties into one core issue: leadership response. Many managers say they want feedback. But when someone speaks up, they bristle. When a staff member challenges a decision, they shut down. When tension arises, they avoid it.
Over time, teams learn to stay quiet. Not because they don’t care. But because pushing back doesn’t feel worth it. And when that happens, everything else starts to decay.
If your team never disagrees, you probably don’t have alignment. You have avoidance. If no one gives feedback, you don’t have trust. You have fear. And if accountability is always top-down, you don’t have ownership. You have compliance.
Fixing this isn’t about more rules or tighter control. It’s about building a culture where feedback is expected, disagreement is valued, and leadership is strong enough to listen.
What Dysfunctional Teams Do
- Stay silent even when something’s wrong
- Avoid conflict to protect themselves
- Agree in meetings, then disengage
- Wait for someone else to take responsibility
- Compete internally instead of collaborating
What Functional Teams Do
- Share concerns early and often
- Disagree respectfully to get better outcomes
- Commit to plans because they had a voice
- Hold each other accountable without blame
- Rally around a shared mission, not personal ego
Final Thoughts: Culture Change Starts with Leadership
The breakdown of a team often starts with silence. But so does its rebuilding. It begins with one leader deciding to listen more, react less, and make it safe to speak. It begins with small shifts: a better question, a recap at the end of a meeting, a moment of vulnerability.
No healthcare team can function well without trust, clarity, ownership, dialogue, and unity. These aren’t soft skills. They’re survival skills. They protect patients, support staff, and strengthen outcomes.
If you’re leading a team, look beyond performance metrics. Pay attention to what people aren’t saying. The absence of feedback, conflict, or disagreement isn’t proof of success. It may be the first sign of dysfunction.
You don’t need to fix it all at once. But you do need to start. Culture is built in the moments between decisions. And every one of those moments is a chance to lead better.
Sources
- Edmondson, A. C. (1999). Psychological safety and learning behavior in work teams. Administrative Science Quarterly, 44(2), 350–383. https://doi.org/10.2307/2666999
- Goleman, D. (2013). Focus: The hidden driver of excellence. Harper.
- Lencioni, P. (2002). The Five Dysfunctions of a Team: A Leadership Fable. Jossey-Bass.
- West, M. A., & Lyubovnikova, J. (2013). Illusions of team working in health care. Journal of Health Organization and Management, 27(1), 134-142. https://doi.org/10.1108/14777261311311843
- Tucker, A. L., & Edmondson, A. C. (2003). Why hospitals don’t learn from failures: Organizational and psychological dynamics that inhibit system change. California Management Review, 45(2), 55–72.