Not Every Answer Lives in the Handbook
Policy is one of the cornerstones of healthcare. In clinical environments where safety, standardization, and compliance drive operations, policies create structure. They define expectations. They reduce variability. They give teams a framework to act within.
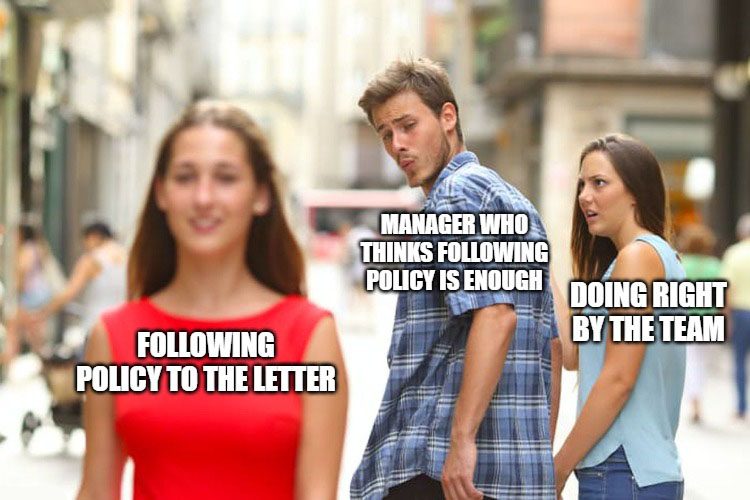
But as important as policy is, it cannot lead.
No policy, no matter how thoughtfully written, can anticipate every situation. No rule can fully account for the unpredictability of human life. Policy was designed to be a guide, not a substitute for leadership. And the moments that define leadership rarely come when everything is working perfectly. They come when the system is strained. When someone who always shows up needs someone else to show up for them.
At Citadel Healthcare Services, we work with healthcare professionals and facilities every day who find themselves at the intersection of policy and reality. What we have learned is simple. Policy is the system. Leadership is the judgment required to make it work.
Join our Leadership Group working towards reshaping healthcare culture. Enjoy Newsletters, Group Discussion, and One-on-One Mentorship.
The Limits of Policy in Clinical Leadership
Healthcare policies exist to safeguard patients, protect employees, and create continuity of care. Scheduling, call-offs, medication administration, reporting structures, credentialing, and documentation are all shaped by policies intended to provide consistency and fairness. From a risk mitigation perspective, policy is essential.
However, the growing complexity of modern healthcare environments has exposed a critical reality. Many policies are built for ideal conditions, yet healthcare rarely operates under those conditions. Emergencies happen. Staffing gaps occur. Human lives intersect with rigid rules, and leaders are often left holding the decision.
A study published in the Journal of Healthcare Leadership observed that nurse managers who interpret policy with judgment, context, and emotional awareness report higher levels of team trust, lower staff turnover, and greater flexibility in managing real-world challenges. The authors note that policy enforcement, in isolation, was often viewed by staff as punitive and disconnected from the realities of bedside care.
When policy is treated as the ceiling instead of the floor, the result is often a demoralized workforce, especially in times of personal crisis. Clinical excellence cannot be achieved through enforcement alone. It must be paired with human-centered leadership.
A Real-World Case: When Policy Cannot Carry the Moment
A nurse who had a reputation for consistency, reliability, and teamwork experienced a last-minute childcare emergency. She called approximately ninety minutes before her night shift, which by facility policy was too late to avoid disciplinary action. The policy required two full hours of notice to avoid a formal write-up.
She did not attempt to excuse herself from responsibility. She was apologetic, stressed, and already seeking coverage options. By the book, she had failed to meet expectations. But when the call was answered, the manager knew immediately this was not about whether the rule had been broken. It was about how the team would respond when the rule no longer applied cleanly to the situation at hand.
Rather than send her into further distress or escalate the issue through disciplinary procedures, the manager stayed. They covered the first four hours of the shift until a casual nurse responded to a short-notice incentive protocol. The floor remained stable. The team adjusted calmly. No one was singled out, and no damage was done.
There was no grand gesture. There was no rewriting of policy. But there was leadership. And what mattered most was what the team saw:
- A stable unit
- A quiet act of support
- A system that held, even when the policy fell short
This decision was not about showing leniency. It was about showing judgment. It was about protecting the culture we were trying to build, not just protecting ourselves from audit risk.
Leadership Judgment as a Strategic Asset
In healthcare, judgment is not a soft skill. It is a leadership essential. The ability to understand a situation in context, weigh the intent behind policy, and respond with clarity separates effective leadership from simple oversight.
Leaders frequently encounter circumstances that policies were never designed to cover. Emergencies, last-minute call-offs, sudden changes in patient acuity, and the personal lives of staff collide with rigid systems meant to provide order. Judgment connects those systems to real-world application. It cannot be automated or reduced to checklists. It requires presence and discernment.
The Agency for Healthcare Research and Quality highlights the link between leadership flexibility and psychological safety. Their findings show that teams led by individuals who respect policy but also respond with situational awareness report concerns earlier, offer feedback more readily, and participate actively in improvement efforts. This responsiveness builds trust, which strengthens communication and cohesion.
The American Organization for Nursing Leadership reports similar outcomes. Leadership practices built on adaptability and emotional intelligence are consistently associated with stronger clinical results. Teams trust leaders who use judgment when pressure is high or when rules do not fit the situation. That trust contributes to engagement, retention, and better patient experiences.
Judgment also supports operational continuity. Automation, float pools, and incentives help, but there are moments when none activate in time. In those cases, a leader’s ability to step in calmly and effectively protects both patient safety and team stability.
Judgment is not simply making exceptions. It is applying the values behind policy in situations where rigid interpretation would cause harm. It is recognizing when the intent of the standard is better served through flexibility and when compassion and accountability must coexist.
Healthcare leadership involves constant unpredictability. The complexity of patient care, scheduling, resource management, and personal circumstances cannot always be captured in written procedures. Leadership judgment transforms a static framework into a functional, supportive system. It keeps people at the center of healthcare, both patients and staff.
Leadership judgment is not a workaround. It is not optional. It is a necessary part of delivering care in environments that are human, demanding, and continually evolving.
Balancing Fairness, Flexibility, and Accountability
A common objection to judgment-driven leadership is the concern that it introduces inconsistency. If one employee is offered flexibility, what prevents others from expecting the same?
The answer lies in transparency and context. Leadership does not mean excusing behavior without accountability. It means evaluating behavior across patterns, past performance, and the intention behind the action. Fairness is not always sameness. In healthcare, where individual team members carry unequal burdens, fairness sometimes means acknowledging those differences.
In the case above, the nurse in question had a long track record of going above and beyond. She was not known for frequent call-offs or policy violations. She had built trust through consistency. Her rare request for support deserved to be weighed in the context of that history.
When leaders act with clarity, document their decisions, and explain the reasoning where appropriate, teams are more likely to accept the nuance without perceiving favoritism. In fact, research published in BMJ Leader found that staff respect for leadership increased when flexibility was applied through structured reflection and open communication.

System Integrity vs. Human Needs
A staffing system must protect operations. But systems must also adapt when the cost of strict application outweighs the benefit. The integrity of the schedule, the staffing grid, and the policy framework is only useful if it can respond to real human needs without collapsing.
Leaders who understand this balance know when to hold the line and when to step over it to protect the very culture the policy was intended to reinforce.
This requires a few key conditions:
- The presence of trust between staff and leadership
- A culture of clear communication around exceptions and rationale
- Written documentation to ensure transparency
- The ability to follow up with improvement planning to avoid recurrence of preventable issues
In our example, we did not make a special policy for childcare emergencies. We documented the variance, communicated the shift changes clearly, and added the event to our next debrief. Leadership was not a substitute for the process. It was the bridge that allowed the process to flex when necessary.
How does your salary and compensation package compare? Get our 2025 Nurse Leader Salary Guide to see!
The Role of Organizational Culture
Policy enforcement becomes much harder in units where trust is thin. When staff feel disconnected, even reasonable decisions can be viewed with suspicion. An exception made for one person might be taken as favoritism by another. Over time, this kind of second-guessing wears down morale. It becomes harder for leaders to act with nuance without causing unintended tension.
But in teams built on trust, culture acts as a stabilizer. Leaders who have shown up with consistency earn room to make difficult calls. Their teams understand that decisions are made with care, not convenience. Even if someone disagrees with the outcome, they are more likely to believe it was made with fairness in mind. That kind of benefit of the doubt does not come automatically. It has to be earned through the way leaders show up, especially when the situation is unclear.
Trust is not built in one meeting or mandated by a policy update. It is shaped in how leaders respond during moments of uncertainty. How they explain their decisions. Whether they are willing to be transparent even when their choices are unpopular. Whether accountability is applied fairly across the board. And whether support and flexibility are reserved for just a few, or offered consistently to those who have proven they deserve it.
Policies absolutely matter. They hold the structure in place and ensure fairness across the system. But there will always be situations that no handbook can cover. Judgment is what fills that gap. And the strength of a team’s culture determines whether that judgment is accepted or challenged. The more grounded the culture, the more space there is for leaders to act wisely, without destabilizing the team in the process.
How Healthcare Leaders Can Embed Flexibility into Policy-Driven Environments
Leadership flexibility must not be accidental. It must be designed.
Here are four key principles for embedding flexibility into policy-guided workplaces:
- Document Variances Properly
Allow leaders to make case-by-case decisions but require proper documentation and follow-up review. This maintains transparency and protects organizational standards. - Train Leaders in Ethical Judgment
Clinical leads, supervisors, and nurse managers should receive scenario-based training in how to navigate gray areas, especially in scheduling, conduct, and performance management. - Communicate Decisions Without Justifying Everything
A brief acknowledgment of the decision, without details that compromise privacy, is often enough to reassure teams that leadership is acting with purpose. - Review Policies for Built-In Discretion
Policies should be reviewed regularly to assess whether rigid enforcement is still serving the intended goals. Building in formal discretion points can help clarify when and how leaders are expected to adapt.
Flexibility is not the enemy of structure. It is the sign that the structure is being led by people, not just maintained by paper.
Join our Leadership Group working towards reshaping healthcare culture. Enjoy Newsletters, Group Discussion, and One-on-One Mentorship.
Implications for Healthcare Recruitment and Retention
Healthcare recruiters know that culture is one of the top three reasons candidates accept or decline offers. In direct placement, particularly in leadership and bedside roles, questions about leadership style, fairness, psychological safety, and team support frequently appear during candidate screening. These are not abstract concerns. Candidates are vetting the environment just as carefully as the facility is vetting them, and many have left previous roles due to leadership gaps, rigid systems, or broken trust.
Facilities that empower their leadership teams to apply discretion, communicate transparently, and lead with trust are more likely to retain their hires. Employees do not want chaos. But they also do not want cold, impersonal systems that treat every exception as a failure. Most healthcare professionals are looking for structure that supports clinical safety, while still allowing room for human judgment and mutual respect in day-to-day operations.
The middle ground is strong leadership.
As staffing partners, we advise our clients to evaluate leadership not only on policy compliance but also on their ability to inspire, support, and retain under real-world conditions. Consistency matters, but so does discretion. Leadership is more than enforcement. It is decision-making under pressure, informed by both standards and context. A facility that cannot adapt in small moments, or that penalizes nuance, will lose big over time. Judgment-based leadership is not a soft skill. It is a strategic advantage that sets high-performing teams apart.
Explore a better leadership search with zero pressure. Pick a free 15 minute slot.
Closing Thoughts
Policy is essential. It creates clarity, fairness, and a shared foundation for decision-making. But no matter how well-crafted, policy was never designed to solve every dilemma a leader will face. There will always be gray areas—moments where the rule is clear, but the right call isn’t. In those spaces, something else has to carry the weight. That’s where leadership steps in.
True leadership is not measured by how accurately someone can quote a handbook. It’s measured by how they lead when the handbook doesn’t have an answer. When the situation is urgent, human, and unresolved by procedure alone.
In those moments, policy becomes a reference. Leadership becomes the tool.
And your team will remember how you led.
Not when everything was perfect, but when it was not.
Not when the answer was easy, but when you chose the right thing anyway.
That’s the part that lives in people’s stories long after the shift is over.
That’s the part that builds culture.
That’s the part that lasts.
Sources:
- American Organization for Nursing Leadership. Nurse Leader Core Competencies. Chicago, IL: AONL. Available at: https://www.aonl.org/resources/nurse-leader-competencies/ AONL+2AONL+2
- American Organization for Nursing Leadership. Nursing Leadership Insight Study – Staffing and Retention Report. Available at: https://www.aonl.org/resources/nursing-leadership-survey AONL
- Agency for Healthcare Research and Quality. Creating Psychological Safety in Teams: Handout. Rockville, MD: AHRQ. Available at: https://www.ahrq.gov/evidencenow/tools/psychological-safety.html AHRQ
- Agency for Healthcare Research and Quality. Annual Perspective: Psychological Safety of Healthcare Staff. Available at: https://psnet.ahrq.gov/perspective/annual-perspective-psychological-safety-healthcare-staff PSNet
- Vu V, et al. How training psychological safety transforms healthcare. PMC. 2025. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC12049904/ PMC
- Negi A, et al. Psychological safety and leadership : Nursing Management. Nursing Management. 2021. Available at: https://journals.lww.com/nursingmanagement/fulltext/2021/11000/psychological_safety_and_leadership.1.aspx LWW Journals
- Majers JS, Warshawsky N. Evidence‑Based Decision‑Making for Nurse Leaders. Nurse Lead. 2020;18(5):471‑475. PMC. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC7388761/ PMC
- Bautista J, et al. An integrative review of leadership competencies and attributes in nursing. PMC. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC6899698/ PMC

