Managing is not enough anymore in nurse leadership. The environment that nurses work in today moves quickly, strains complex systems, and demands more than control and compliance can hold together. We have entered a new era of nurse leadership and the old playbook is crumbling. Leadership built on silence, hierarchy, and defensiveness doesn’t only feel out of date- it pushes good clinicians away. The result is a widening gap between what patients need and what teams have the energy and clarity to deliver.
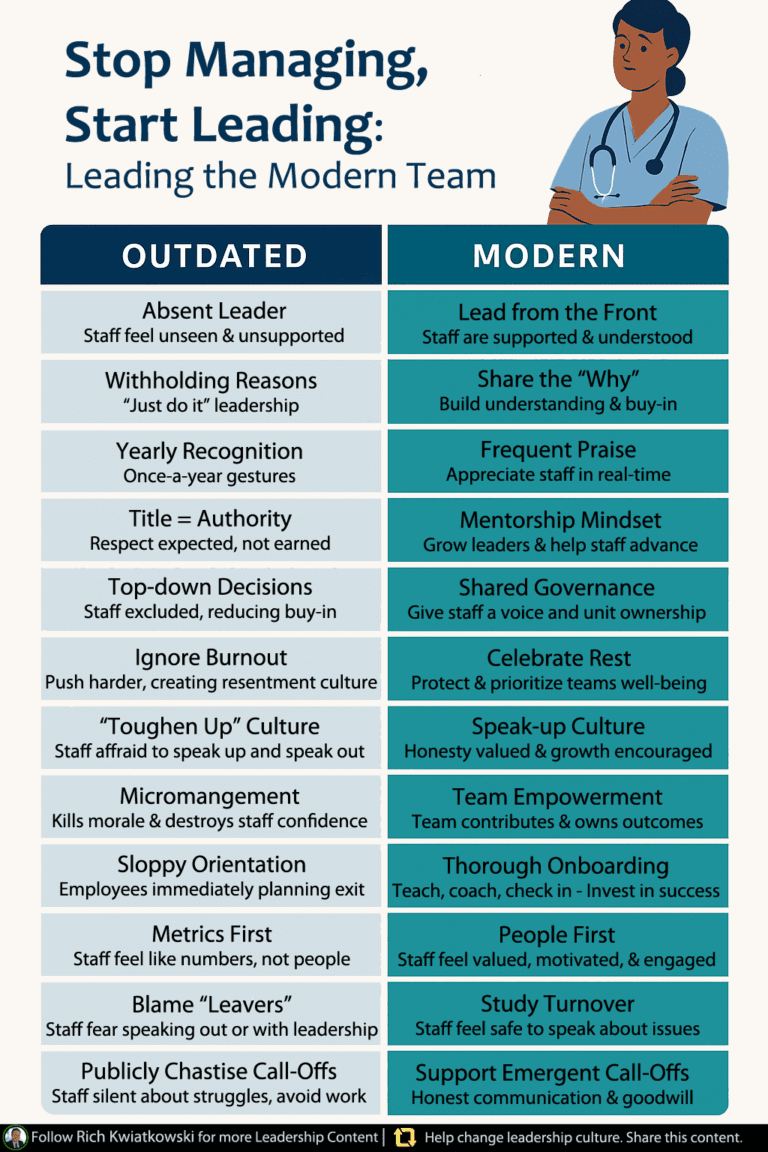
Teams don’t need more tough love, more blanket policies, or more memos that explain everything except the reason a decision was made. Staff benefit from leaders who are visible and present. The most effective approach explains the why, teaches and coaches, recognizes effort in real time, and builds systems that protect rest and learning rather than drain both. A healthy culture makes it safe to raise a concern, admit an error, ask for help, and offer an idea that improves care. In short, mentors matter more than managers, and structures should make the right thing the easy thing.
Over the last year I reviewed guidance, videos, and articles from patient safety organizations, health care leadership institutes, nurse residency programs, and practice scholars. A handful of themes emerged with striking consistency. Each theme has a trickle down effect. When leaders adopt it, the climate of the unit changes and with it the experience of care and the probability that a great nurse will stay. The five themes are simple to name and demanding to live. Be visible and engaged. Explain the why. Recognize frequently and mentor rather than micromanage. Create a speak up culture rooted in a just approach to error. Protect rest and build onboarding that sets people up to succeed. The remainder of this article unpacks those themes and shows how they translate into daily leadership choices that strengthen the culture.
Get our 2025 Nurse Salary Guide
The Culture You Have is the Behavior You Model
Culture doesn’t live in the handbook. It lives in the daily experience of people at work. That experience is shaped first and most by how leaders show up. When leaders spend time on the unit, ask about difficulties and resources, and close the loop on what they hear, the signal to staff is that it’s safe to speak and that concerns matter. This is not a soft claim. Leader rounds that are consistent and purposeful are associated with better safety climate and proactive risk reduction. Teams feel more comfortable surfacing problems, which allows those problems to be addressed before they become harm to patients or staff. The presence of leadership acts as a catalyst for shared awareness and reliability across disciplines and shifts.1,2
Leadership style also cascades directly into outcomes. Approaches that mirror transformational leadership principles are linked with stronger safety culture, better nurse outcomes, and better patient outcomes. Leaders who create a compelling direction, who empower, and who support growth, cultivate engagement and ownership. When the default interaction is coaching rather than commanding, you see more initiative, better teamwork, and fewer costly workarounds.3,4
Recognition and trust deserve their own space in this conversation. High quality recognition, offered frequently and tied to specific behaviors and values, is one of the most reliable levers for retention. People who feel seen are less likely to leave. Teams that trust their leaders are more willing to bring forward a concern and to follow through on improvement efforts. Consistency and sincerity matter more than ceremony. A short, specific thank you given at the right moment is more powerful than an annual award that arrives months after the effort. 5,6
With that context set, let us move from principles to practice and explore the five themes in depth.
Theme One: Be Visible & Engaged
The foundation of a healthy culture in nurse leadership is the everyday presence of leadership in the work.. That does not mean hovering or inspecting. It means listening, learning, and removing obstacles. When a manager rounds consistently with intent, two things happen. First, staff experience leadership as accessible and accountable. Second, leaders get unfiltered data from the point of care and can make grounded decisions quickly.
A practical way to build this habit is to establish a weekly leadership walk. Treat it as an appointment you do not cancel. During each leadership round:
- Ask what is getting in the way of safe care today.
- Ask for one small fix that could be in place by next week.
- Ask what support from leadership is missing.
Capture answers on the spot and commit to one actionable follow up per round. Close the loop at the next huddle by reporting what changed because the concern was raised. The act of returning with the update is where trust is built. Once that cycle repeats, people believe that speaking up is worth the time and that leadership is a partner rather than a judge. Structured rounds of this kind are associated with stronger safety climate because they normalize honest discussion of risk and build a shared language for improvement. 1
Presence also changes how information flows. Many units rely on stand ups that are long on announcements and short on dialogue. Shift the purpose. Treat the huddle as a brief exchange that surfaces safety signals, staffing pinch points, and near miss learnings. Rotate facilitation so that different voices lead. When the same two people speak at every huddle, psychological safety for the rest of the team doesn’t grow. When a novice speaks and is thanked for raising a concern, everyone notices.
Make the work of improvement visible. Keep a simple public backlog that shows issues, owners, and due dates. Visibility is a form of respect. It tells the team that their concerns are not disappearing into a black box. It also reduces the rumor mill that builds when people have to guess what is being done and by whom.
The deeper point is that presence is not performative. It’s productive. You will find hazards earlier, hear ideas sooner, coach in the moment, and build credibility one loop closure at a time. That credibility is the currency you will need when a difficult change must move quickly.
Curious what a top-down, culture-first search could do for your unit? Schedule a call today
Theme Two: Explain the Why
Effective nurse leadership explains the why behind decisions, which prevents frustration and builds ownership.. Human motivation research explains why this happens. People are more likely to internalize a change and persist with it if they understand the rationale, feel they have some autonomy within it, and believe they can be competent at it. This is the logic of self determination theory and it applies as much to a seasoned charge nurse as it does to a student. 7
Clarity about the why is also a trust accelerator. When leaders communicate transparently about performance, constraints, and trade offs, trust increases even when the news is difficult. Responsible transparency is not about releasing everything you know. It’s about sharing useful context at the right time, committing to follow through, and inviting input that can still influence the plan. In today’s environment, trust is a competitive advantage. Teams who trust their leaders are more willing to try something new, to voice dissent before rollout, and to sustain the change once launched. 8,9
Adopt a standard script for changes. Begin with the reason this is needed now. Tie it to safety signals, regulatory requirements, staffing trends, or patient outcomes. Then describe what will change with precision. If it is a pilot, state that and name the date on which you will review the results. Outline how you will support people with training, tools, and time. Finish with a clear place for feedback and a date for reassessment.
Invite dissent early. Ask two or three frontline voices to pressure test a change before rollout. When you incorporate a suggestion, credit the person by name during the announcement. That acknowledgment encourages others to offer input in the future. Over time, your team will begin to preempt the question by explaining the why to one another, which is a sign that the habit has taken root.
When urgency is high and time is short, you can still explain why. A one minute why at the start of a huddle reframes a policy as a patient safety action, connects it to observed risks, and reinforces respect for people’s time.
Theme Three: Top Nurse Leaders Frequently Recognize & Mentor, Don’t Micromanage
Within nurse leadership, recognition and mentorship can look like soft skills, yet they drive retention and capability.. Data from large cross industry analyses show that meaningful, frequent recognition reduces quit risk in the following months and years. Teams that get recognition right see higher engagement and lower voluntary turnover. The effect is strongest when recognition is timely, specific, linked to values, and inclusive rather than reserved for a few stars. 5 In nursing practice, programs that celebrate meaningful recognition, such as the DAISY Award, are associated with healthier work environments and stronger engagement. 6
Micromanagement, by contrast, slowly erodes initiative and confidence. Leaders who coach and mentor replace control with growth. Mentorship improves job satisfaction, competence, and confidence, especially for early career nurses who are navigating complex environments while still building clinical judgment. Coaching style leadership that supports autonomy and growth is emerging as a powerful retention lever for the modern workforce. 10,11,12
Turn this theme into practice with three habits:
- Establish a recognition rhythm that privileges the everyday moment. At the end of a shift or during a huddle, offer a short thanks that names the behavior and its impact.
- Track recognition coverage each month. The goal is not the count of kudos. The goal is the percentage of the team that received meaningful recognition.
- Build mentorship beyond precepting. Pair new or transitioning nurses with trained mentors for six to twelve months and publish shared goals.
Coaching in one to one check ins can be simple. The GROW model is effective because it’s short and respectful. Ask about the goal, discuss the current reality, explore options together, and close with one small next step the nurse owns. When people experience that pattern repeatedly, they begin to bring options rather than problems. That is culture change in action.
Theme Four: Create a Speak Up Culture with a Just Approach to Problems & Mistakes
Psychological safety in nurse leadership means it’s safe to ask questions, raise concerns, and report near misses. Psychological safety is not optional. It’s linked to better learning, better problem solving, better adaptability, and better patient outcomes, particularly in high risk settings where coordination and clear voice matter most. Contemporary reviews and healthcare focused analyses continue to affirm this relationship. 13,14
A just culture is the operating system that supports psychological safety. In a just culture, the response to error is balanced and focused on learning. It distinguishes among human error, at risk behavior, and reckless behavior, and it responds differently to each. It pairs accountability with support and focuses on systems that set people up for success. A just culture never confuses punishment with improvement. National patient safety resources offer practical training and case studies for leaders who want to make this shift. 15
Leadership presence helps here as well. When leaders conduct rounds that invite open conversation about hazards and near misses and close the loop by showing what changed, they model the response the organization values. Over time, staff learn that raising a concern is not a career risk. It’s how work gets safer. 1
Make the change visible in your language. Replace the reflexive question of who made the error with a better question that seeks to understand how the system set people up for the miss and what will be changed by the end of the week. Follow incidents and near misses with short debriefs that collect the facts, identify contributing factors, name one change, and end with one appreciation for what someone did well under pressure. Provide a low friction way to raise concerns anonymously, and invest equal effort in building a climate where people are comfortable raising concerns directly. Post a weekly update that shows what the unit said and what leadership did.
Measurement helps. Use a validated safety culture survey and focus on domains that track communication openness and nonpunitive response to error. Track your responses over time and link them to the reliability of safety practices on your unit. 16
Get our 2025 Nurse Salary Guide
Theme Five: Protect Rest & Build Systems for Sustainable Nurse Leadership. Onboard Like You Mean It.
The fastest way to undermine a good culture is to ignore fatigue and treat call offs as character flaws. Burnout and sleep loss are not only hard on clinicians. They harm patients. A recent systematic review and meta analysis found that nurse burnout is associated with lower care quality, lower safety, and lower patient satisfaction. Fatigue and extended shifts raise error risk. Night and rotating shifts carry higher risk as well. Twelve hour shifts can work for some teams, but they require guardrails for coverage and recovery if you want to avoid the hazards tied to fatigue. 17,18,19
Presenteeism deserves specific attention. Working while unwell increases risk to patients and to colleagues. The literature describes cultural pressures that push people to show up sick, especially where staffing is tight. Leaders who support emergent call offs treat fitness for duty as a safety requirement rather than a moral failing. This shift is essential if you want to reduce harm and sustain staffing. 20
On the positive side, strong onboarding and transition to practice programs reduce early tenure turnover and improve confidence and competence. National nurse residency programs report higher first year retention than prevailing averages, and studies show that thoughtful orientation upgrades move retention year over year. An effective onboarding plan is not a welcome packet. It’s a ninety day roadmap with clear competencies, mentor check ins, and moments that surface and address psychological safety. 21, 22
Translate this theme into practice with a few clear commitments:
- Define a rest standard and protect it with coverage. Aim for an uninterrupted meal break and scheduled short breaks on long shifts, with proactive float support.
- Put guardrails around back to back overtime and monitor meal break compliance as a safety metric.
- Create a respectful protocol for emergent call offs. Use a simple script for fitness for duty, centralize backfill through staffing, and review patterns monthly for root causes.
- Launch a visible ninety day onboarding plan for every new nurse. Publish mentor assignments, meeting cadence, and skill milestones.
Weekly new hire huddles can surface friction points you would otherwise only hear about during an exit interview. Charge nurses can check in at predictable times in the shift to spot fatigue and move coverage. Quiet, consistent actions in these areas build trust faster than any slogan.
Summary
It’s not enough to just be visible- you have to be engaged so that trust and safety climate grow from daily interactions rather than speeches. Explain the why so that people internalize changes and put their energy into the work instead of guessing the rationale. Recognize frequently and replace micromanagement with mentorship so that capability and confidence expand across the team. Create a speak up culture with a just approach to error so that learning accelerates and risks are addressed early. Protect rest and build onboarding that helps people succeed in the first ninety days so that the team you invested in doesn’t burn out or walk away. Each theme reinforces the others. Together they create a climate where excellent nurses choose to stay.
Bring your toughest leadership role—we’ll show you our approach. Schedule a call today

Turning the Ideas Into a Thirty Day Practice Sprint
Many leaders ask how to begin without waiting for perfect conditions. Begin with what you control and start small enough that consistency is possible.
- Week one. Schedule a weekly walk and listen round and keep that appointment. Ask about barriers, ask for one small fix, and ask what support is missing. Return with one update that closes the loop. Add a simple anonymous concern link and commit to reviewing submissions on a set day.
- Week two. Use the same short script for every change that begins with the reason for the change. Offer a specific recognition every day and invite peers to share a shout out at the next huddle.
- Week three. Publish your rest standard and protect it with coverage. Measure breaks taken and celebrate progress. Share one story about a respectful emergent call off handled well.
- Week four. Pair each new or transitioning team member with a mentor and publish a ninety day plan on one page that both can see. End the month with a short reflection on what changed and what should be improved next month.
While this sprint won’t fix everything, it will demonstrate leaderships seriousness and begin to alter expectations. When you follow through on small promises week after week, you build the credibility required to tackle bigger issues such as staffing ratios, equipment reliability, or interdepartmental communication.
Common Pushbacks & Grounded Responses
A common objection is that there isn’t time for formal recognition. However, the reality is that you don’t have time for turnover. A specific thank you that links behavior to impact takes seconds and compounds into loyalty over time. Analyses show that meaningful recognition materially lowers the risk that people will leave. 5
Another objection claims that explaining the why invites debate that slows execution. Providing rationale increases internalization and reduces the policing you will have to do later. It also strengthens trust, which allows teams to move quickly when it matters.7,9
A third concern is that sick time is abused and strictness is necessary. Presenteeism is frequently a bigger risk than absenteeism in clinical environments. It increases errors, transmission risk, and recovery time. Supporting emergent call offs with clear process and respect is a safety practice.20
Skeptics sometimes say that leader rounds are performative. They become performative only when leaders fail to close the loop. When rounds are structured, and follow through is public, the safety climate improves and staff engagement rises because people believe their voice can lead to change.1
Shared Governance & Magnet Principles Multiply the Impact
If you want nurses to act like owners with buy-in, give them formal avenues to own decisions. Shared governance models bring staff into choices about practice, equipment, and policy. Magnet frameworks translate the idea into a structure that many hospitals use to stabilize culture and improve results. The core ideas are familiar by now. Transformational leadership. Structural empowerment. Exemplary professional practice. New knowledge and innovation. Clear outcomes. Whether or not your organization pursues formal recognition, the practices that underpin these frameworks help units recruit, retain, and grow. 23,24,25
If you don’t have formal shared governance on your unit, begin with a practice council that meets monthly. Select one practice standard to review and improve each month. Publish minutes and outcomes. Rotate facilitators. Over time you will build confidence and evidence that frontline voice leads to better decisions and better results.
Leaders Self-Check
Take five quiet minutes and answer these questions honestly.
- Do your staff know why your top three unit priorities matter.
- When was the last time you changed course because staff raised a concern and you told the story publicly.
- Can you name three people you recognized this week and exactly what they did.
- Do new nurses on your unit have named mentors and a ninety day plan you can see on one page.
- Could a nurse on nights safely say pause, I am concerned, and be thanked for it.
If your answer is “not yet” to most of these, consider that a starting line rather than a failure. Culture is a set of repeated choices. Begin repeating the right ones.
A Ninety Day Culture Plan
In the first month, focus on visibility and voice. Round weekly with intent, publish a “Simple Issues & Actions” board, and open an anonymous concern link while you work to make anonymity unnecessary. In the second month, focus on clarity and coaching. Use the same short script for every change and maintain a steady recognition rhythm. Pair people with mentors and schedule quick coaching conversations that end with one action owned by the clinician. In the third month, focus on rest and onboarding. Publish your rest standard and keep it. Launch a visible ninety day onboarding plan for every new nurse. Hold a brief new hire huddle each week to surface friction and remove it. At the end of the ninety days, pulse your safety culture survey on the domains you targeted, review first year retention for the quarter, and look for early movement in outcomes tied to reliability on your unit. Expect noise. Continue anyway.
Reduce time to fill and keep great leaders longer. Schedule a call today.
Final Word
The best nurse leadership avoids creating dependency. They build trust, clarity, and momentum. They are visible. They explain the why. They recognize frequently and coach for growth. They invite voice and adopt a just response to error. They protect rest and onboard like they mean it. When you lead that way, you don’t have to persuade great staff to stay. They stay because the culture makes sense and because it makes them better clinicians, and ultimately makes care safer. Begin with one small promise to your team this week and keep it. Culture will follow.
Sources
- Institute for Healthcare Improvement. Patient Safety Leadership WalkRounds.
- Executive and Leader Walk Rounds for High Reliability. BMJ Open Quality.
- AHRQ PSNet. Leadership, Safety Climate, and Continuous Quality Improvement.
- Boamah S et al. Transformational Leadership and Nurse Outcomes.
- Gallup. Employee Retention Depends on Getting Recognition Right.
- Lippincott. The DAISY Award and Healthy Work Environments.
- Advances in Simulation. Applying Self Determination Theory in Health Professions Education.
- Deloitte. Transparency at Work as a Trust Accelerator.
- Research on trust in leadership and work quality among health workers.
- Sigma Nursing publications on mentorship and nurse retention.
- American Nurse Journal. Coaching Leadership for Nurse Retention.
- Reviews on coaching style leadership and autonomy support in nursing.
- Annual Review of Organizational Psychology and Organizational Behavior. Psychological Safety.
- Narrative and systematic reviews of psychological safety in health care teams.
- AHRQ CUSP. Just Culture Training and Case Modules.
- AHRQ. Surveys on Patient Safety Culture and the Workplace Safety Item Set.
- JAMA Network Open. Nurse Burnout and Patient Outcomes.
- AHRQ PSNet. Fatigue, Sleep Deprivation, and Patient Safety Primer.
- Reviews on extended shifts, fatigue, and safety risks in nursing.
- Integrative reviews and AHRQ perspectives on presenteeism in health care.
- American Association of Colleges of Nursing and Vizient. Nurse Residency Program Fact Sheet.
- Program pages describing residency structure, transition to practice, and outcomes.
- NCBI Bookshelf. Magnet Frameworks and Shared Governance overview.
- Academic and practice articles on structural empowerment and shared governance.
- Case reports linking Magnet principles to retention and outcomes.