If you’ve led a hospital unit for more than a minute, you’ve felt the gut-punch that follows an assault on a nurse. The charge board doesn’t just list rooms anymore; it lights up with all the places your system is thin. In the aftermath, policy memos fly and inboxes fill. But the real solution doesn’t live in a PDF. It lives on the floor- shift to shift, room to room- where nurses, techs, physicians, and security either act like a team or act like strangers.
This article makes a simple, evidence-based case: a high-trust floor culture is the most reliable antidote to patient-to-nurse violence. Yes, you’ll still need security, de-escalation training, and compliance with standards. But the daily micro-behaviors and leadership presence on your unit are where prevention either takes root or dies. We’ll walk through what a floor culture that reduces patient-to-nurse violence actually looks like (in plain language), how to align it with today’s regulatory expectations, and how to prove the ROI to your CFO without breaking a sweat.
Along the way, we’ll keep this SEO core phrase front and center: patient-to-nurse violence– because calling the problem by its name helps the right readers find the right solutions.
The Uncomfortable Baseline: Why patient-to-nurse violence is still rising
Let’s start by naming the scope. Health care workers make up roughly a tenth of the U.S. workforce but experience nearly half of all nonfatal workplace-violence injuries that lead to days away from work. In 2021–2022, the nonfatal injury rate in health care was more than triple the all-industry rate. That’s not a rounding error; that’s an epidemic inside the workforce that cares for everyone else. CDC Blogs
Patient-to-nurse violence isn’t just a safety issue; it’s a business issue. The American Hospital Association (AHA) pegs the 2023 cost of violence to U.S. hospitals at $18.27 billion, including prevention and response- every training hour, every security upgrade, every medical bill tied to an assault. If your organization treats patient-to-nurse violence as “unfortunate but inevitable,” you’re paying for it twice: once in human harm and again in cash. American Hospital Association
Regulators have moved, too. The Joint Commission’s workplace-violence prevention standards (effective January 1, 2022) require leadership accountability, data collection, reporting systems, training, and post-event strategies. You’re expected to run a real prevention program, not a binder. Joint Commission International
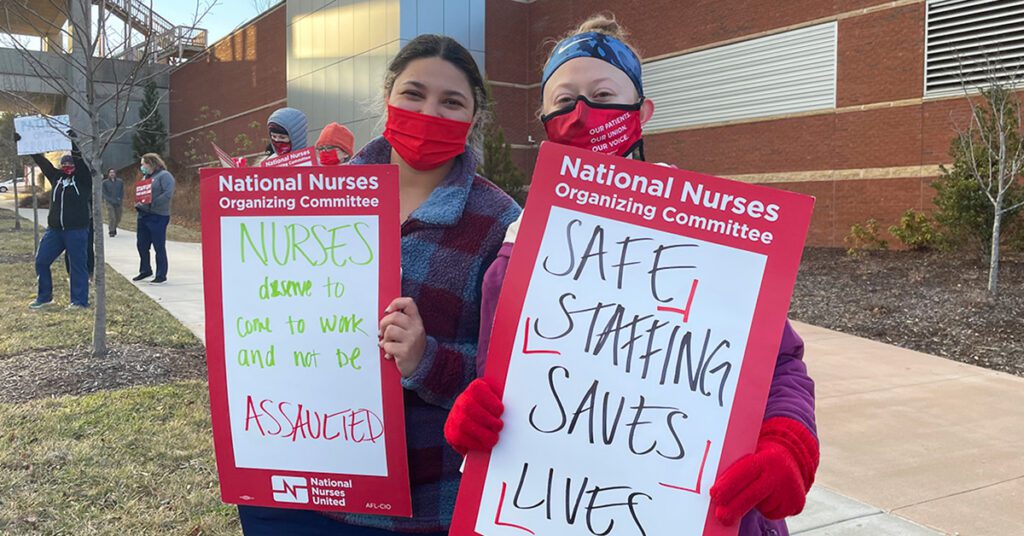
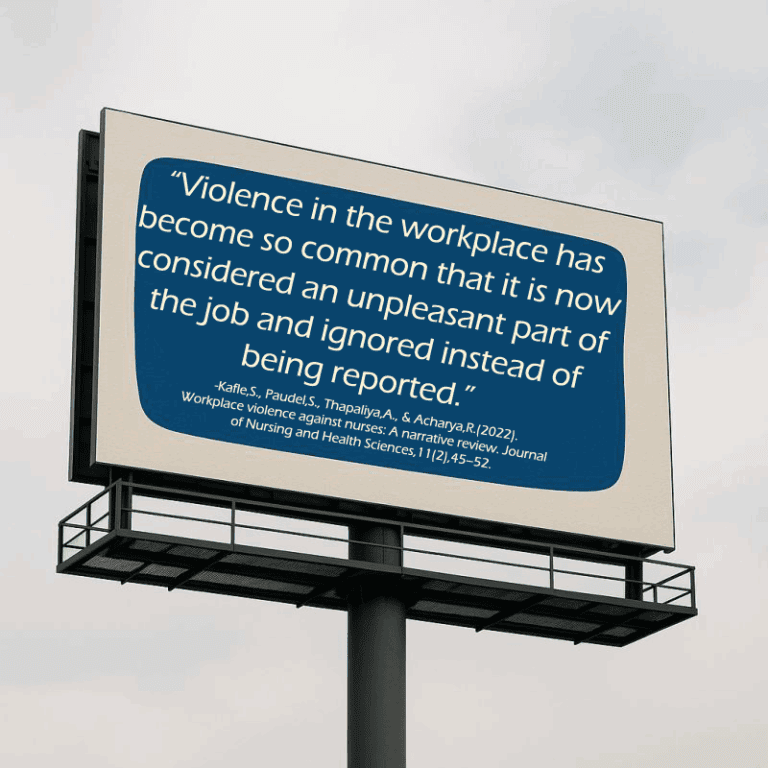
Meanwhile, OSHA is advancing toward a dedicated standard for health care and social assistance. Even before a final rule, OSHA already cites the General Duty Clause and publishes detailed guidance. Translation: expectations are climbing, and patient-to-nurse violence can no longer be waved away as “part of the job.” OSHA
And then there’s underreporting. The silent accelerant of patient-to-nurse violence. Nurses routinely skip reporting because the process is clunky, they doubt anything will change, or they fear being blamed. When leaders don’t fix the loop, the data go dark and so do the budgets that depend on them. ANA
Join our Leadership Group working towards reshaping healthcare culture. Enjoy Newsletters, Group Discussion, and One-on-One Mentorship.
What Actually Works: The four pillars of a floor culture that prevents patient-to-nurse violence
You can’t chant your way to culture. You build it in consistent, observable habits. Four pillars distinguish floors that bend the curve on patient-to-nurse violence:
- Predictive practice (see escalation early)
- Tight teamwork (shared words and roles under stress)
- Visible leadership (leaders in the room, not just in the recap)
- Relentless learning (incidents → insight → change)
Each pillar maps to research-backed moves you can start in the next 30 days.

Pillar 1: Predictive Practice: See it before it spikes
Patient-to-nurse violence is often preceded by patterns. Units that avoid injuries don’t “go with a feeling”; they screen and signal.
Use a brief, validated risk screen. The Brøset Violence Checklist (BVC) takes about 30 seconds and predicts near-term risk. Recent studies, including a 2025 analysis and prior multisite work, support its short-window predictive value in inpatient settings. The point isn’t to label patients; it’s to trigger protective behaviors when scores cross a threshold. PMC
Pair BVC with STAMP cues in real time. STAMP (Staring, Tone, Anxiety, Mumbling, Pacing) gives busy clinicians a quick, shared language to recognize escalating behavior during routine care. It’s simple, memorable, and built from front-line observation. PubMed
Make the signal visible. When BVC or STAMP indicates higher risk, physically flag the room on the charge board and in the huddle script. Evidence shows that EHR “behavioral flags” alone are imperfect- nurses value the heads-up but worry about bias and inconsistent follow-through- so tie any flag to specific, time-boxed actions (buddy-in, security awareness, shortened encounter). JAMA Network
This is how predictive practice shrinks patient-to-nurse violence: not by predicting the future perfectly, but by buying time. Time to buddy up, de-escalate early, and call help before you’re already behind. PMC
How does your salary and compensation package compare? Get our 2025 Nurse Leader Salary Guide to see!
Pillar 2: Tight Teamwork: Shared words, shared moves
On units that reliably prevent patient-to-nurse violence, teamwork under stress isn’t a vibe; it’s a script.
Adopt TeamSTEPPS 3.0 language and make it muscle memory. CUS (“I’m Concerned, Uncomfortable, this is a Safety issue.”) and SBAR handoffs give teams a common shorthand when seconds count. AHRQ’s 2023 refresh of TeamSTEPPS ties these tools to workforce well-being- because teamwork skills reduce confusion and burnout while improving safety. Practice the words in your space, not in a classroom miles away. AHRQ
Design the buddy system like a clinical order, not a suggestion. “Buddy required” should be automatic at a given BVC score or STAMP pattern and auditable on the board. When the rule is fuzzy, it disappears at 3 a.m.
Create one place to defuse safely. Even a low-cost “quiet room” (clear exits, no entrapment angles, line of sight to hall) gives teams somewhere to de-escalate without escalating to restraint. This is not about aesthetics; environment design is prevention. Hospitals are already spending billions on safety infrastructure; start where behavior actually happens. American Hospital Association
Teamwork becomes real when a leader can see it at a glance: the board shows who’s the buddy, huddles use consistent words, and staff know exactly where to move a conversation before it turns into patient-to-nurse violence.
Pillar 3: Visible Leadership: Be in the room, not just the review
Floors that reduce patient-to-nurse violence don’t wait for debriefs to bring leaders to the bedside. Leaders staff the second for high-risk rooms when staffing is tight; they take the first 90 seconds of a hot conversation; they close the loop after every alert with “what we changed,” not just “thanks for reporting.”
This is bigger than good manners. It’s culture signaling- authentic leadership in the AACN Healthy Work Environment model- and it’s tied to lower burnout and better retention. Patient-to-nurse violence and nurse attrition feed each other; strong, present leadership weakens both. AHRQ
If you need the business case, it’s painful but clear: average RN turnover now costs around $61,000 per nurse, and that’s before you account for the reputational and survey risks when patient-to-nurse violence hits the news. Prevent the injuries and you prevent the exits. NSI Nursing Solutions

Pillar 4: Relentless Learning: Incidents become improvement, fast
Everyone says they value learning. Floors that actually reduce patient-to-nurse violence write it into the rhythm of the work.
Fix reporting first. If filing a violence report takes more than two minutes, you’re accidentally encouraging silence. Build a one-minute pathway with pre-filled fields and a checkbox taxonomy. Then guarantee a 72-hour response that shows the action taken (moved the vitals cart, tightened the buddy rule, adjusted the huddle script). Underreporting thrives where feedback dies. ANA
Stand up a Behavioral Emergency Response Team (BERT). A cross-disciplinary team comprised of behavioral health, unit RN’s, trained security, and social work (as available), reduces assaults, reduces restraint use, and increases staff satisfaction when activated early on clear criteria. Patient-to-nurse violence drops when your floor knows who to call before a code. PMC
Run a 15-minute “violence huddle” once a month. Share three numbers (incidents, near-misses, BERT calls), one story, and one change you’re testing. When you document this cadence, you’re not just improving; you’re also demonstrating compliance with The Joint Commission’s expectations for data, oversight, and improvement. Joint Commission International
The cycle is simple: screen → signal → support → study → strengthen. When that loop is visible, patient-to-nurse violence becomes a system problem you manage, not a storm you weather.
Curious what a top-down, culture-first search could do for your unit? Schedule a no-commitment, free call today!
Make it real in 30 days (no extra FTEs required)
Leaders often ask, “Where do I start?” Start on the floor. Here’s a compact plan you can execute with the team you have. We’ll say “patient-to-nurse violence” out loud because that’s the workplace harm you’re targeting.
Week 1: Baseline and signals.
Pick your risk tool (BVC). Write a 10-minute huddle script that calls out high-risk rooms and assigns buddies by name. Put a visible icon on the board for any room flagged that shift. Run a two-minute practice on leaving the room safely if tone escalates. Patient-to-nurse violence often spikes when staff feel trapped; practice the exit. PMC
Week 2: Shared words and roles.
Roll out TeamSTEPPS CUS and SBAR for behavioral handoffs. Name one “de-escalator” per shift- a nurse or tech who can float for 10 minutes when a situation warms. Test your panic alert and log response times. Patient-to-nurse violence thrives in ambiguity; shared words cut the fog. AHRQ
Week 3: BERT and reporting.
Publish BERT activation criteria aligned to your BVC thresholds and STAMP cues. Cut your reporting clicks in half and place the link on every workstation. Promise a 72-hour “what we changed” note. Patient-to-nurse violence becomes less “normal” when reporting becomes normal. PMC
Week 4: Leadership and layout.
Leaders staff the second for every flagged room this week. Walk the unit with facilities and fix two environmental traps (line-of-sight blind spots, furniture that creates entrapment angles). Hold your first 15-minute violence huddle: three numbers, one story, one change. Patient-to-nurse violence is physical; your fixes should be, too. American Hospital Association
At the end of 30 days, you won’t have solved patient-to-nurse violence. But you will have installed a floor-level prevention system that your team can feel.
Align With Standards, Win Resources
Your culture work should double as compliance. Map your floor practices to the Joint Commission’s requirements: leadership oversight (leaders staffing the second), policies and training (TeamSTEPPS + BERT criteria), reporting and data (one-minute pathway + monthly huddle), and post-event strategies (72-hour change notes). That’s not just safer; it’s survey-ready. Joint Commission Digital Assets
For budget season, lead with the AHA numbers: $18.27B in violence-related costs across U.S. hospitals in 2023. Pair that with your unit’s RN turnover math (roughly $61,110 per RN on average) and you’ve reframed spending on prevention as a margin-saving investment. Patient-to-nurse violence drains talent and cash; prevention returns both. American Hospital Association
And keep an eye on the federal landscape. As OSHA advances a dedicated standard, organizations that treat patient-to-nurse violence as a continuous-improvement focus- not a paperwork obligation- will be miles ahead. OSHA
Hard Truths About Flags, Training, and “Part of the job”
A few realities leaders should acknowledge out loud:
EHR behavioral flags are not a force field. Nurses appreciate a heads-up, but flags can be inconsistently applied and can mirror broader inequities (studies have found disparities by race and insurance status). If you use flags, time-limit them, require renewal criteria, and, most important, tie them to specific actions (buddy-in, security aware, shortened encounters). Patient-to-nurse violence declines when flags prompt behaviors, not bias. JAMA Network
Annual, four-hour de-escalation trainings don’t change the floor. Confidence and skill improve when practice is short, specific, and recurring in the real space where care occurs. Convert one long class into quarterly 20-minute micro-sessions. Patient-to-nurse violence is situational; your training should be, too. (TeamSTEPPS materials and pocket guides help you standardize language.) AHRQ
“It’s part of the job” is the fastest way to normalize harm. Underreporting is driven by clunky processes and a belief that nothing changes. When you shorten the clicks and close the loop with visible improvements, reporting rises, and with it your credibility and your data to fund fixes. ANA
The Human Side: Well-being as a control measure
Healthy work environments don’t just feel better; they buffer risk. Protect meal breaks with buddy coverage. Normalize same-day access to EAP or peer support after an assault and schedule a follow-up within 72 hours. Map one AACN Healthy Work Environment standard per quarter to your violence-prevention work- e.g., “skilled communication” → de-escalation scripts and TeamSTEPPS refreshers. Safer people de-escalate better, and better de-escalation reduces patient-to-nurse violence. AHRQ
Talking Points for Executives (use them as written)
- “Patient-to-nurse violence is costing us twice- once in staff injuries and again in turnover. AHA estimates $18.27B nationally; our RN turnover averages ~$61k each. A modest investment in floor culture is a cost-avoidance strategy.” American Hospital Association
- “Our plan aligns directly with The Joint Commission’s standards: leadership presence, data and reporting, training, and post-event action. We’ll be able to show surveyors our learning loop in action.” Joint Commission Digital Assets
- “OSHA is moving toward a formal standard. Installing this now reduces regulatory risk later.” OSHA
When executives see that your floor culture strategy targets patient-to-nurse violence with measurable steps and recognized frameworks, resources follow.
What Success Looks Like (On Your Unit)
You’ll know the culture has shifted when you can walk the floor at 2 p.m. or 2 a.m. and witness the same things:
- The charge board marks high-risk rooms with a standard icon; buddies are named, not implied.
- Huddles sound the same across shifts. Brief, specific behavioral handoffs using CUS and SBAR.
- The “quiet space” is known, available, and used early.
- A BERT page brings the right people in under five minutes- and often earlier, because staff call sooner.
- One-minute incident reports get filed in the moment, not at end of shift, and staff receive a short “what we changed” note within 72 hours.
- The monthly violence huddle shares three numbers, one story, and one change. No blame, just improvement.
That’s what a prevention culture looks like. And that’s how you turn down the volume on patient-to-nurse violence without waiting for a miracle budget or a perfect census.
Final Word to Leaders
The worst moment after an assault is the question that shouldn’t have to be asked: “What could you have done differently?” On floors where leaders are present, language is shared, and learning is relentless, the better question is automatic: “What did we learn about our system, and what will we change by Friday?”
Patient-to-nurse violence is not part of the job. It’s a system risk you can manage. Start on the floor. Start this month. And don’t stop.
References
- Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. (2024, May 29). Prioritizing our healthcare workers: The importance of addressing the intersection of workplace violence and mental health and wellbeing. NIOSH Science Blog. https://blogs.cdc.gov/niosh-science-blog/2024/05/29/hcw_violence_mh/
- American Hospital Association. (2025, March). The burden of violence to U.S. hospitals (Research report). https://www.aha.org/system/files/media/file/2025/05/The-Burden-of-Violence-to-US-Hospitals.pdf
- The Joint Commission. (2021, June 18). R3 Report, Issue 30: Workplace violence prevention standards (effective January 1, 2022). https://www.jointcommission.org/en-us/standards/r3-report/r3-report-30/
- Occupational Safety and Health Administration. (n.d.). Healthcare: Workplace violence. https://www.osha.gov/healthcare/workplace-violence
- Occupational Safety and Health Administration. (n.d.). Preventing workplace violence in healthcare. https://www.osha.gov/hospitals/workplace-violence
- American Nurses Association. (2024). Unreported workplace violence—Why is this so common? https://www.nursingworld.org/content-hub/resources/workplace/unreported-workplace-violence—why-is-this-so-common/
- Hvidhjelm, J., Nielsen, B., Nielsen, A. C., & Høegh, M. C. (2025). Predictive validity of the Brøset Violence Checklist in a large, routine clinical dataset. Journal of Intellectual Disability Research, 69(7), 786–798. https://doi.org/10.1111/jir.13233
- Kös, T., Rognli, E. W., Løberg, E.-M., Møller, P., & Rypdal, K. (2024). The predictive validity of the V-RISK-10 and BVC among psychiatric inpatients: A multicentre prospective cohort study. Frontiers in Psychiatry, 15, 1342445. https://doi.org/10.3389/fpsyt.2024.1342445
- Spencer, C., Hughes, M., & Patel, R. (2024). Psychometric analysis of the Brøset Violence Checklist in medical–surgical nursing units. Nursing Forum, 59(4), 1234–1245. https://onlinelibrary.wiley.com/doi/full/10.1155/nuf/5574982
- Luck, L., Jackson, D., & Usher, K. (2007). STAMP: Components of observable behaviour that indicate potential for patient violence in emergency departments. Journal of Advanced Nursing, 59(1), 11–19. https://pubmed.ncbi.nlm.nih.gov/17543010/
- Seeburger, E. F., Gonzales, R., South, E. C., O’Neill, G., Blecker, S., & Agarwal, A. K. (2023). Qualitative perspectives of emergency nurses on electronic health record behavioral flags to promote workplace safety. JAMA Network Open, 6(4), e239057. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2803958
- Agarwal, A. K., Seeburger, E. F., O’Neill, G., South, E. C., & Blecker, S. (2023). Prevalence of behavioral flags in the electronic health record among Black and White patients visiting the emergency department. JAMA Network Open, 6(1), e2251734. https://pubmed.ncbi.nlm.nih.gov/36656576/
- Dahnke, D., & Mulkey, M. A. (2021). Using a behavioral response team on non-psychiatric nursing units. MEDSURG Nursing, 30(4), 229–233. https://pmc.ncbi.nlm.nih.gov/articles/PMC10181858/
- Rajwani, A., Clark, N., & Montalvo, C. (2023). Understanding best practices in implementation of behavioral emergency response teams through a scoping review. Journal of the American Psychiatric Nurses Association, 29(6), 465–478. https://pubmed.ncbi.nlm.nih.gov/35918889/
- Bruccoli, A. M. (2023). Implementation of a behavioral emergency response team in the emergency department. Journal of Emergency Nursing, 49(3), 395–402. https://doi.org/10.1016/j.jen.2023.01.011
- Agency for Healthcare Research and Quality. (2023–2024). TeamSTEPPS® 3.0 (Program hub and curriculum). https://www.ahrq.gov/teamstepps-program/index.html
- Agency for Healthcare Research and Quality. (2022). Surveys on Patient Safety Culture® (SOPS®): Workplace safety supplemental items for hospitals. https://www.ahrq.gov/sops/surveys/hospital/supplemental-items/workplace-safety.html
- NSI Nursing Solutions, Inc. (2025). 2025 National Health Care Retention & RN Staffing Report. https://www.nsinursingsolutions.com/documents/library/nsi_national_health_care_retention_report.pdf
- American Association of Critical-Care Nurses. (2025). Healthy work environments (HWE) standards and resources. https://www.aacn.org/nursing-excellence/healthy-work-environments

Mary Hinton
Hey there! I’ve been following your weblog for some time now and finally got the bravery to go ahead and give you a shout out from Austin Texas! Just wanted to say keep up the fantastic work!